Kidney and Nephron Physiology - MCAT Biology
Card 0 of 20
The main function of the Loop of Henle is to __________.
The main function of the Loop of Henle is to __________.
The main function of the Loop of Henle is to establish a concentration gradient so that water can be reabsorbed from the collecting duct and avoid being lost as urine. Although the ascending limb does absorb water, this water would be lost as urine if it were not for the concentration gradient established in the medulla of the kidney. Neither sodium nor potassium is absorbed in the Loop of Henle.
The main function of the Loop of Henle is to establish a concentration gradient so that water can be reabsorbed from the collecting duct and avoid being lost as urine. Although the ascending limb does absorb water, this water would be lost as urine if it were not for the concentration gradient established in the medulla of the kidney. Neither sodium nor potassium is absorbed in the Loop of Henle.
Compare your answer with the correct one above
Which of the following is true regarding the nephron?
Which of the following is true regarding the nephron?
Together, Bowman's capsule and the glomerulus make up the renal corpuscle. Blood flows through the glomerulus, where high hydrostatic pressures force plasma through the fenestrations of the glomerular endothelium into Bowman's capsule. The substance that ends up in the capsule is called the filtrate, which then moves to the proximal tubule. Proteins, glucose, and ions are secreted from the proximal tubule back into the blood.
The collecting duct is impermeable to water and is not particularly sensitive to aldosterone. Instead, aldosterone, a steroid hormone produced by the adrenal cortex, acts primarily at the distal tubule to increase sodium reabsorption, potassium secretion, and ultimately water reabsorption to increase blood pressure. The distal tubule absorbs Na+ and Ca2+, not HCO3-.
Together, Bowman's capsule and the glomerulus make up the renal corpuscle. Blood flows through the glomerulus, where high hydrostatic pressures force plasma through the fenestrations of the glomerular endothelium into Bowman's capsule. The substance that ends up in the capsule is called the filtrate, which then moves to the proximal tubule. Proteins, glucose, and ions are secreted from the proximal tubule back into the blood.
The collecting duct is impermeable to water and is not particularly sensitive to aldosterone. Instead, aldosterone, a steroid hormone produced by the adrenal cortex, acts primarily at the distal tubule to increase sodium reabsorption, potassium secretion, and ultimately water reabsorption to increase blood pressure. The distal tubule absorbs Na+ and Ca2+, not HCO3-.
Compare your answer with the correct one above
What of the following are not involved in the flow of filtrate through nephrons?
What of the following are not involved in the flow of filtrate through nephrons?
The correct path of filtrate through a nephron starts in the renal corpuscle, which is comprised of the glomerulus and Bowman's capsule. Filtrate then passes through the proximal convoluted tubule, where the majority of reabsorption takes place. It then travels through the descending and ascending limbs of the Loop of Henle, creating the counter current multiplier gradient that will allow urine to be concentration in the collecting duct. From the Loop of Henle, filtrate enters the distal convoluted tubule for final reabsorption before entering the collecting duct and being trasported to the bladder.
The renal artery is used to carry blood into the kidneys. Filtrate originates from the renal artery, but it is not a part of the nephrons.
The correct path of filtrate through a nephron starts in the renal corpuscle, which is comprised of the glomerulus and Bowman's capsule. Filtrate then passes through the proximal convoluted tubule, where the majority of reabsorption takes place. It then travels through the descending and ascending limbs of the Loop of Henle, creating the counter current multiplier gradient that will allow urine to be concentration in the collecting duct. From the Loop of Henle, filtrate enters the distal convoluted tubule for final reabsorption before entering the collecting duct and being trasported to the bladder.
The renal artery is used to carry blood into the kidneys. Filtrate originates from the renal artery, but it is not a part of the nephrons.
Compare your answer with the correct one above
Which of the following processes occurs in the kidney?
Which of the following processes occurs in the kidney?
The kidney uses all three of the following processes: filtration, secretion and reabsorption. All three of these processes aid in allowing the body to filter waste products from the blood while retaining nutrients, salts, and water when needed.
Filtration occur when filtrate is separated from blood in the renal corpuscle. Reabsorption is the removal of ions from the filtrate to retain salts. Secretion is the input of salts to the filtrate to eliminate them. All of these processes occur in the nephrons.
The kidney uses all three of the following processes: filtration, secretion and reabsorption. All three of these processes aid in allowing the body to filter waste products from the blood while retaining nutrients, salts, and water when needed.
Filtration occur when filtrate is separated from blood in the renal corpuscle. Reabsorption is the removal of ions from the filtrate to retain salts. Secretion is the input of salts to the filtrate to eliminate them. All of these processes occur in the nephrons.
Compare your answer with the correct one above
What is the main function of the Loop of Henle within each nephron?
What is the main function of the Loop of Henle within each nephron?
The Loop of Henle creates a countercurrent multiplier system. As the filtrate descends through the Loop of Henle, water leaves the filtrate and is reabsorbed, making the filtrate very concentrated. When the Loop of Henle ascends, salt ions leave the filtrate and are reabsorbed making the filtrate less concentrated. This creates a strong concentration of ions in the interstitial fluid toward the bottom of the loop, as compared to the concentration at the top. When filtrate flows down the collecting duct, this gradient helps concentrate the urine by removing water.
The Loop of Henle creates a countercurrent multiplier system. As the filtrate descends through the Loop of Henle, water leaves the filtrate and is reabsorbed, making the filtrate very concentrated. When the Loop of Henle ascends, salt ions leave the filtrate and are reabsorbed making the filtrate less concentrated. This creates a strong concentration of ions in the interstitial fluid toward the bottom of the loop, as compared to the concentration at the top. When filtrate flows down the collecting duct, this gradient helps concentrate the urine by removing water.
Compare your answer with the correct one above
Which of the following is most directly responsible for concentrating urine in the kidney?
Which of the following is most directly responsible for concentrating urine in the kidney?
The ascending and descending limbs of the Loop of Henle are responsible for creating a countercurrent multiplier system, which concentrates urine and allows water and electrolytes to passively diffuse down their concentration gradients.
All the other options are part of the nephron, but are not responsible for the process of urine concentration. The glomerulus and Bowman's capsule are responsible for collecting and producing initial filtrate from the blood, and form the renal corpuscle. The proximal convoluted tuble is the initial site of reabsorption.
The ascending and descending limbs of the Loop of Henle are responsible for creating a countercurrent multiplier system, which concentrates urine and allows water and electrolytes to passively diffuse down their concentration gradients.
All the other options are part of the nephron, but are not responsible for the process of urine concentration. The glomerulus and Bowman's capsule are responsible for collecting and producing initial filtrate from the blood, and form the renal corpuscle. The proximal convoluted tuble is the initial site of reabsorption.
Compare your answer with the correct one above
A renal afferent arteriole has a larger radius than the efferent arteriole. What is the effect of this larger radius on the function of the kidney?
A renal afferent arteriole has a larger radius than the efferent arteriole. What is the effect of this larger radius on the function of the kidney?
A renal afferent arteriole is directed toward the glomerulus, while a renal efferent arteriole is directed away from the glomerlus. If the radius of the afferent arteriole is increased, there is more flow through it toward the glomerulus, and if there is a smaller radius in the efferent arteriole, there is a resultant back pressure in the glomerulus. This is can be imagined as trying to squeeze a high-pressure hose through a small pipe. This pressure increases the force within the glomerulus to increase filtration, and subsequently increase reabsorption.
Antidiuretic hormone (ADH) secretion has a neglible effect on the radius of renal arterioles. Blood flow to the kidney is increased when afferent arteriole radius is increased (this also increases the arteriole flow).
A renal afferent arteriole is directed toward the glomerulus, while a renal efferent arteriole is directed away from the glomerlus. If the radius of the afferent arteriole is increased, there is more flow through it toward the glomerulus, and if there is a smaller radius in the efferent arteriole, there is a resultant back pressure in the glomerulus. This is can be imagined as trying to squeeze a high-pressure hose through a small pipe. This pressure increases the force within the glomerulus to increase filtration, and subsequently increase reabsorption.
Antidiuretic hormone (ADH) secretion has a neglible effect on the radius of renal arterioles. Blood flow to the kidney is increased when afferent arteriole radius is increased (this also increases the arteriole flow).
Compare your answer with the correct one above
Which of the following sections of the nephron does not change the osmolarity of the filtrate?
Which of the following sections of the nephron does not change the osmolarity of the filtrate?
The purpose of the proximal tubule is to reduce the amount of filtrate in the nephron. The proximal tubule does alter the solute concentrations in the filtrate, but it does not alter the osmolarity of the filtrate. This is because the proximal tubule is where reabsorption of solutes, proteins, and glucose takes place. Meanwhile, drugs and toxins are being secreted into the filtrate. Essentially, the volume of filtrate in the proximal tubule decreases, but the filtrate remains isotonic to the blood.
The purpose of the proximal tubule is to reduce the amount of filtrate in the nephron. The proximal tubule does alter the solute concentrations in the filtrate, but it does not alter the osmolarity of the filtrate. This is because the proximal tubule is where reabsorption of solutes, proteins, and glucose takes place. Meanwhile, drugs and toxins are being secreted into the filtrate. Essentially, the volume of filtrate in the proximal tubule decreases, but the filtrate remains isotonic to the blood.
Compare your answer with the correct one above
At which point in a nephron would the osmolarity of the filtrate be highest? Assume that antidiuretic hormone (ADH) is not present in the body.
At which point in a nephron would the osmolarity of the filtrate be highest? Assume that antidiuretic hormone (ADH) is not present in the body.
It is important to understand how urine is concentrated as it travels through the nephron. The proximal convoluted tubule does not alter the osmolarity of the filtrate, the loop of Henle increases the osmolarity of the filtrate, and the distal convoluted tubule lowers the osmolarity of the filtrate. In the absence of antidiuretic hormone, the collecting duct will be impermeable to water, preventing it from leaving the filtrate and resulting in more dilute urine. With the collecting duct impermeable to water, the filtrate will be most concentrated at the bottom of the loop of Henle.
It is important to understand how urine is concentrated as it travels through the nephron. The proximal convoluted tubule does not alter the osmolarity of the filtrate, the loop of Henle increases the osmolarity of the filtrate, and the distal convoluted tubule lowers the osmolarity of the filtrate. In the absence of antidiuretic hormone, the collecting duct will be impermeable to water, preventing it from leaving the filtrate and resulting in more dilute urine. With the collecting duct impermeable to water, the filtrate will be most concentrated at the bottom of the loop of Henle.
Compare your answer with the correct one above
The interaction between blood pressure and kidney function in humans requires coordination by the renin-angiotensin-aldosterone system (RAAS). This system involves the dynamic interplay of the kidneys, lungs, and blood vessels to carefully regulate sodium and water balance.
A normal human kidney has cells adjacent to the glomerulus called juxtaglomerular cells. These cells sense sodium content in urine of the distal convoluted tubule, releasing renin in response to a low level. Renin is an enzyme that converts angiotensinogen to angiotensin I (AI). AI is converted to angiotensin II (AII) by angiotensin converting enzyme (ACE) in the lung.
AII stimulates aldosterone secretion in the zona glomerulosa of the adrenal gland. Aldosterone then acts to upregulate the sodium-potassium pump on the basolateral side of distal tubule epithelial cells to increase sodium reabsorption from the urine, as well as increasing potassium excretion.
A scientist is studying the effect of aldosterone on the distal tubule cells of a kidney. He finds that antidiuretic hormone also exerts changes on the concentration of urine produced by this kidney. Where does antidiuretic hormone exert its most potent effect?
The interaction between blood pressure and kidney function in humans requires coordination by the renin-angiotensin-aldosterone system (RAAS). This system involves the dynamic interplay of the kidneys, lungs, and blood vessels to carefully regulate sodium and water balance.
A normal human kidney has cells adjacent to the glomerulus called juxtaglomerular cells. These cells sense sodium content in urine of the distal convoluted tubule, releasing renin in response to a low level. Renin is an enzyme that converts angiotensinogen to angiotensin I (AI). AI is converted to angiotensin II (AII) by angiotensin converting enzyme (ACE) in the lung.
AII stimulates aldosterone secretion in the zona glomerulosa of the adrenal gland. Aldosterone then acts to upregulate the sodium-potassium pump on the basolateral side of distal tubule epithelial cells to increase sodium reabsorption from the urine, as well as increasing potassium excretion.
A scientist is studying the effect of aldosterone on the distal tubule cells of a kidney. He finds that antidiuretic hormone also exerts changes on the concentration of urine produced by this kidney. Where does antidiuretic hormone exert its most potent effect?
Antidiuretic hormone (ADH), also known as vasopressin, increases the permeability of the collecting duct to water. This allows a more concentrated urine to be excreted, because water is being lost from the urine to the kidney tissue before excretion. The gradient created by the reabsorption of ions from the loop of Henle means that the interstitium is hypertonic to the collecting duct. If the permeability of the collecting duct to water is increased, we would expect water to flow out of the collecting duct. We would expect ADH levels to increase with dehydration in order to preserve water.
Antidiuretic hormone (ADH), also known as vasopressin, increases the permeability of the collecting duct to water. This allows a more concentrated urine to be excreted, because water is being lost from the urine to the kidney tissue before excretion. The gradient created by the reabsorption of ions from the loop of Henle means that the interstitium is hypertonic to the collecting duct. If the permeability of the collecting duct to water is increased, we would expect water to flow out of the collecting duct. We would expect ADH levels to increase with dehydration in order to preserve water.
Compare your answer with the correct one above
The interaction between blood pressure and kidney function in humans requires coordination by the renin-angiotensin-aldosterone system (RAAS). This system involves the dynamic interplay of the kidneys, lungs, and blood vessels to carefully regulate sodium and water balance.
A normal human kidney has cells adjacent to the glomerulus called juxtaglomerular cells. These cells sense sodium content in urine of the distal convoluted tubule, releasing renin in response to a low level. Renin is an enzyme that converts angiotensinogen to angiotensin I (AI). AI is converted to angiotensin II (AII) by angiotensin converting enzyme (ACE) in the lung.
AII stimulates aldosterone secretion in the zona glomerulosa of the adrenal gland. Aldosterone then acts to upregulate the sodium-potassium pump on the basolateral side of distal tubule epithelial cells to increase sodium reabsorption from the urine, as well as increasing potassium excretion.
Aldosterone functions by increasing the rate at which the sodium-potassium pump functions in the basolateral surface of distal tubule epithelial cells of the nephron. Which of the following is true of the sodium-potassium pump?
The interaction between blood pressure and kidney function in humans requires coordination by the renin-angiotensin-aldosterone system (RAAS). This system involves the dynamic interplay of the kidneys, lungs, and blood vessels to carefully regulate sodium and water balance.
A normal human kidney has cells adjacent to the glomerulus called juxtaglomerular cells. These cells sense sodium content in urine of the distal convoluted tubule, releasing renin in response to a low level. Renin is an enzyme that converts angiotensinogen to angiotensin I (AI). AI is converted to angiotensin II (AII) by angiotensin converting enzyme (ACE) in the lung.
AII stimulates aldosterone secretion in the zona glomerulosa of the adrenal gland. Aldosterone then acts to upregulate the sodium-potassium pump on the basolateral side of distal tubule epithelial cells to increase sodium reabsorption from the urine, as well as increasing potassium excretion.
Aldosterone functions by increasing the rate at which the sodium-potassium pump functions in the basolateral surface of distal tubule epithelial cells of the nephron. Which of the following is true of the sodium-potassium pump?
The sodium-potassium pump pumps three sodium ions out of the cytosol, and two potassium ions into the cytosol. It is electrogenic because each sodium and potassium ion have a charge of positive one, and the two ions are pumped in unequal quantities. The pump generates an electric gradient and current due to the directional flow of positive charge out of the cell.
When aldosterone is released, it increases the action of the sodium-potassium pump, causing excess sodium to be removed from the filtrate in the distal tubule, thus conserving sodium and drawing water out of the filtrate.
The sodium-potassium pump pumps three sodium ions out of the cytosol, and two potassium ions into the cytosol. It is electrogenic because each sodium and potassium ion have a charge of positive one, and the two ions are pumped in unequal quantities. The pump generates an electric gradient and current due to the directional flow of positive charge out of the cell.
When aldosterone is released, it increases the action of the sodium-potassium pump, causing excess sodium to be removed from the filtrate in the distal tubule, thus conserving sodium and drawing water out of the filtrate.
Compare your answer with the correct one above
The interaction between blood pressure and kidney function in humans requires coordination by the renin-angiotensin-aldosterone system (RAAS). This system involves the dynamic interplay of the kidneys, lungs, and blood vessels to carefully regulate sodium and water balance.
A normal human kidney has cells adjacent to the glomerulus called juxtaglomerular cells. These cells sense sodium content in urine of the distal convoluted tubule, releasing renin in response to a low level. Renin is an enzyme that converts angiotensinogen to angiotensin I (AI). AI is converted to angiotensin II (AII) by angiotensin converting enzyme (ACE) in the lung.
AII stimulates aldosterone secretion in the zona glomerulosa of the adrenal gland. Aldosterone then acts to upregulate the sodium-potassium pump on the basolateral side of distal tubule epithelial cells to increase sodium reabsorption from the urine, as well as increasing potassium excretion.
The passage notes that the RAAS functions at the distal tubule. What is the primary function of the proximal tubule?
The interaction between blood pressure and kidney function in humans requires coordination by the renin-angiotensin-aldosterone system (RAAS). This system involves the dynamic interplay of the kidneys, lungs, and blood vessels to carefully regulate sodium and water balance.
A normal human kidney has cells adjacent to the glomerulus called juxtaglomerular cells. These cells sense sodium content in urine of the distal convoluted tubule, releasing renin in response to a low level. Renin is an enzyme that converts angiotensinogen to angiotensin I (AI). AI is converted to angiotensin II (AII) by angiotensin converting enzyme (ACE) in the lung.
AII stimulates aldosterone secretion in the zona glomerulosa of the adrenal gland. Aldosterone then acts to upregulate the sodium-potassium pump on the basolateral side of distal tubule epithelial cells to increase sodium reabsorption from the urine, as well as increasing potassium excretion.
The passage notes that the RAAS functions at the distal tubule. What is the primary function of the proximal tubule?
The proximal tubule is the primary site of solute reabsorption and secretion, modifying the urine after its initial filtration in the glomerulus.
Concentration of the filtrate primarily occurs in the collecting duct, and the distal convoluted tubule transports urine from the loop of Henle to the collecting duct. Filtration occurs in the glomerulus and Bowman's capsule, know together as the renal corpuscle.
The proximal tubule is the primary site of solute reabsorption and secretion, modifying the urine after its initial filtration in the glomerulus.
Concentration of the filtrate primarily occurs in the collecting duct, and the distal convoluted tubule transports urine from the loop of Henle to the collecting duct. Filtration occurs in the glomerulus and Bowman's capsule, know together as the renal corpuscle.
Compare your answer with the correct one above
The interaction between blood pressure and kidney function in humans requires coordination by the renin-angiotensin-aldosterone system (RAAS). This system involves the dynamic interplay of the kidneys, lungs, and blood vessels to carefully regulate sodium and water balance.
A normal human kidney has cells adjacent to the glomerulus called juxtaglomerular cells. These cells sense sodium content in urine of the distal convoluted tubule, releasing renin in response to a low level. Renin is an enzyme that converts angiotensinogen to angiotensin I (AI). AI is converted to angiotensin II (AII) by angiotensin converting enzyme (ACE) in the lung.
AII stimulates aldosterone secretion in the zona glomerulosa of the adrenal gland. Aldosterone then acts to upregulate the sodium-potassium pump on the basolateral side of distal tubule epithelial cells to increase sodium reabsorption from the urine, as well as increasing potassium excretion.
The first place that early urine is collected after filtration in the glomerulus is which of the following?
The interaction between blood pressure and kidney function in humans requires coordination by the renin-angiotensin-aldosterone system (RAAS). This system involves the dynamic interplay of the kidneys, lungs, and blood vessels to carefully regulate sodium and water balance.
A normal human kidney has cells adjacent to the glomerulus called juxtaglomerular cells. These cells sense sodium content in urine of the distal convoluted tubule, releasing renin in response to a low level. Renin is an enzyme that converts angiotensinogen to angiotensin I (AI). AI is converted to angiotensin II (AII) by angiotensin converting enzyme (ACE) in the lung.
AII stimulates aldosterone secretion in the zona glomerulosa of the adrenal gland. Aldosterone then acts to upregulate the sodium-potassium pump on the basolateral side of distal tubule epithelial cells to increase sodium reabsorption from the urine, as well as increasing potassium excretion.
The first place that early urine is collected after filtration in the glomerulus is which of the following?
Bowman's capsule collects fluid filtered from the glomerulus and serves as a site of entry into the proximal tubule. The glomerulus is a convoluted capillary bed adjacent to Bowman's capsule. Osmotic and oncotic pressure gradients work to filter the blood from the glomerulus into Bowman's capsule. The nature of the epithelial cells that line the glomerulus determines the permeability of the filtration, and prevents unwanted content in the urine.
Filtrate moves from Bowman's capsule to the proximal tubule and into the loop of Henle, which dives into the renal medulla before returning to the renal cortex. From the loop of Henle, filtrate is transferred to the distal tubule and into the collecting duct, where it travels into the renal medulla for collection.
Bowman's capsule collects fluid filtered from the glomerulus and serves as a site of entry into the proximal tubule. The glomerulus is a convoluted capillary bed adjacent to Bowman's capsule. Osmotic and oncotic pressure gradients work to filter the blood from the glomerulus into Bowman's capsule. The nature of the epithelial cells that line the glomerulus determines the permeability of the filtration, and prevents unwanted content in the urine.
Filtrate moves from Bowman's capsule to the proximal tubule and into the loop of Henle, which dives into the renal medulla before returning to the renal cortex. From the loop of Henle, filtrate is transferred to the distal tubule and into the collecting duct, where it travels into the renal medulla for collection.
Compare your answer with the correct one above
The interaction between blood pressure and kidney function in humans requires coordination by the renin-angiotensin-aldosterone system (RAAS). This system involves the dynamic interplay of the kidneys, lungs, and blood vessels to carefully regulate sodium and water balance.
A normal human kidney has cells adjacent to the glomerulus called juxtaglomerular cells. These cells sense sodium content in urine of the distal convoluted tubule, releasing renin in response to a low level. Renin is an enzyme that converts angiotensinogen to angiotensin I (AI). AI is converted to angiotensin II (AII) by angiotensin converting enzyme (ACE) in the lung.
AII stimulates aldosterone secretion in the zona glomerulosa of the adrenal gland. Aldosterone then acts to upregulate the sodium-potassium pump on the basolateral side of distal tubule epithelial cells to increase sodium reabsorption from the urine, as well as increasing potassium excretion.
A nephrologist is studying a normal glomerulus, and notes that it is actively filtering blood normally. What type of blood vessels comprise the bulk of the glomerulus?
The interaction between blood pressure and kidney function in humans requires coordination by the renin-angiotensin-aldosterone system (RAAS). This system involves the dynamic interplay of the kidneys, lungs, and blood vessels to carefully regulate sodium and water balance.
A normal human kidney has cells adjacent to the glomerulus called juxtaglomerular cells. These cells sense sodium content in urine of the distal convoluted tubule, releasing renin in response to a low level. Renin is an enzyme that converts angiotensinogen to angiotensin I (AI). AI is converted to angiotensin II (AII) by angiotensin converting enzyme (ACE) in the lung.
AII stimulates aldosterone secretion in the zona glomerulosa of the adrenal gland. Aldosterone then acts to upregulate the sodium-potassium pump on the basolateral side of distal tubule epithelial cells to increase sodium reabsorption from the urine, as well as increasing potassium excretion.
A nephrologist is studying a normal glomerulus, and notes that it is actively filtering blood normally. What type of blood vessels comprise the bulk of the glomerulus?
The main purpose of the glomerulus is filtration; thus, it is mainly composed of the thinnest walled-blood vessels (capillaries), and specifically those with pores (fenestrations) to facilitate filtration.
The main purpose of the glomerulus is filtration; thus, it is mainly composed of the thinnest walled-blood vessels (capillaries), and specifically those with pores (fenestrations) to facilitate filtration.
Compare your answer with the correct one above
The interaction between blood pressure and kidney function in humans requires coordination by the renin-angiotensin-aldosterone system (RAAS). This system involves the dynamic interplay of the kidneys, lungs, and blood vessels to carefully regulate sodium and water balance.
A normal human kidney has cells adjacent to the glomerulus called juxtaglomerular cells. These cells sense sodium content in urine of the distal convoluted tubule, releasing renin in response to a low level. Renin is an enzyme that converts angiotensinogen to angiotensin I (AI). AI is converted to angiotensin II (AII) by angiotensin converting enzyme (ACE) in the lung.
AII stimulates aldosterone secretion in the zona glomerulosa of the adrenal gland. Aldosterone then acts to upregulate the sodium-potassium pump on the basolateral side of distal tubule epithelial cells to increase sodium reabsorption from the urine, as well as increasing potassium excretion.
A nephrologist is studying a glomerulus, and notes that it is actively filtering blood normally. Which of the following blood vessels contributes most to maintaining appropriate pressure in the glomerulus?
The interaction between blood pressure and kidney function in humans requires coordination by the renin-angiotensin-aldosterone system (RAAS). This system involves the dynamic interplay of the kidneys, lungs, and blood vessels to carefully regulate sodium and water balance.
A normal human kidney has cells adjacent to the glomerulus called juxtaglomerular cells. These cells sense sodium content in urine of the distal convoluted tubule, releasing renin in response to a low level. Renin is an enzyme that converts angiotensinogen to angiotensin I (AI). AI is converted to angiotensin II (AII) by angiotensin converting enzyme (ACE) in the lung.
AII stimulates aldosterone secretion in the zona glomerulosa of the adrenal gland. Aldosterone then acts to upregulate the sodium-potassium pump on the basolateral side of distal tubule epithelial cells to increase sodium reabsorption from the urine, as well as increasing potassium excretion.
A nephrologist is studying a glomerulus, and notes that it is actively filtering blood normally. Which of the following blood vessels contributes most to maintaining appropriate pressure in the glomerulus?
The glomerulus is a capillary bed. Afferent arterioles carry blood to enter the glomerulus, and efferent arterioles carry blood away from the glomerulus after filtration. Both types of arteriole are able to tighten and relax to modulate pressure within the glomerulus, driving filtration. Though fenestrated capillaries form the glomerulus itself, these vessels cannot regulate flow and pressure because they have no smooth muscle.
The glomerulus is a capillary bed. Afferent arterioles carry blood to enter the glomerulus, and efferent arterioles carry blood away from the glomerulus after filtration. Both types of arteriole are able to tighten and relax to modulate pressure within the glomerulus, driving filtration. Though fenestrated capillaries form the glomerulus itself, these vessels cannot regulate flow and pressure because they have no smooth muscle.
Compare your answer with the correct one above
The interaction between blood pressure and kidney function in humans requires coordination by the renin-angiotensin-aldosterone system (RAAS). This system involves the dynamic interplay of the kidneys, lungs, and blood vessels to carefully regulate sodium and water balance.
A normal human kidney has cells adjacent to the glomerulus called juxtaglomerular cells. These cells sense sodium content in urine of the distal convoluted tubule, releasing renin in response to a low level. Renin is an enzyme that converts angiotensinogen to angiotensin I (AI). AI is converted to angiotensin II (AII) by angiotensin converting enzyme (ACE) in the lung.
AII stimulates aldosterone secretion in the zona glomerulosa of the adrenal gland. Aldosterone then acts to upregulate the sodium-potassium pump on the basolateral side of distal tubule epithelial cells to increase sodium reabsorption from the urine, as well as increasing potassium excretion.
A scientist is studying a normally functioning nephron in an adult human. He examines the filtrate as it moves through the ascending limb of the loop of Henle. What observation is he most likely to make?
The interaction between blood pressure and kidney function in humans requires coordination by the renin-angiotensin-aldosterone system (RAAS). This system involves the dynamic interplay of the kidneys, lungs, and blood vessels to carefully regulate sodium and water balance.
A normal human kidney has cells adjacent to the glomerulus called juxtaglomerular cells. These cells sense sodium content in urine of the distal convoluted tubule, releasing renin in response to a low level. Renin is an enzyme that converts angiotensinogen to angiotensin I (AI). AI is converted to angiotensin II (AII) by angiotensin converting enzyme (ACE) in the lung.
AII stimulates aldosterone secretion in the zona glomerulosa of the adrenal gland. Aldosterone then acts to upregulate the sodium-potassium pump on the basolateral side of distal tubule epithelial cells to increase sodium reabsorption from the urine, as well as increasing potassium excretion.
A scientist is studying a normally functioning nephron in an adult human. He examines the filtrate as it moves through the ascending limb of the loop of Henle. What observation is he most likely to make?
The ascending limb of the loop of Henle is permeable to salt, not water. As salt is removed from the urine, the urine becomes less concentrated. The urine will ultimately be concentrated in the collecting duct prior to excretion. The ascending limb of the loop of Henle helps to establish the salt gradient of the nephron, ensuring that water will be removed from the urine as it travels down the collecting duct, ultimately increasing the final concentration, even by decreasing the immediate concentration.
The ascending limb of the loop of Henle is permeable to salt, not water. As salt is removed from the urine, the urine becomes less concentrated. The urine will ultimately be concentrated in the collecting duct prior to excretion. The ascending limb of the loop of Henle helps to establish the salt gradient of the nephron, ensuring that water will be removed from the urine as it travels down the collecting duct, ultimately increasing the final concentration, even by decreasing the immediate concentration.
Compare your answer with the correct one above
Hypersensitivity reactions occur when body tissues are affected by an abnormal immune reaction. The result is damage to normal tissues and clinical illness. A peanut allergy is an example of a hypersensitivity reaction, but there are three additional broad classes.
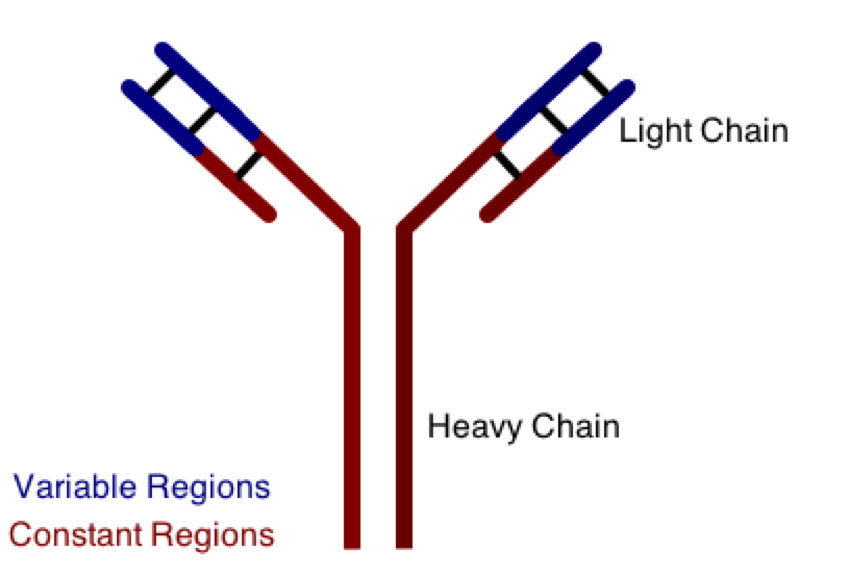
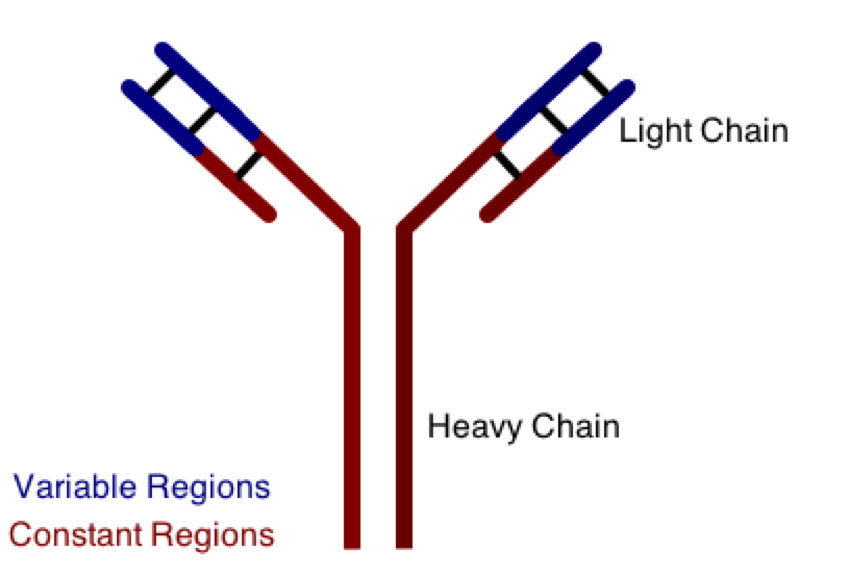
One class involves the abnormal production or deposition of antibodies. Antibodies are B-cell derived molecules that normally adhere to pathogens, rendering them unable to continue an infection. When antibodies are produced against normal tissues, however, disease can result. Figure 1 depicts a schematic structure of an antibody.
Antibodies can be divided into two peptide chains: heavy and light. Heavy chains form the backbone of the antibody, and are attached to light chains via covalent bonding. Each heavy and light chain is then further divided into constant and variable regions. Variable regions exhibit molecular variety, generating a unique chemical identity for each antibody. These unique patterns help guarantee that the body can produce antibodies to recognize many possible molecular patterns on invading pathogens.
In hypersensitivity reactions, antibodies can complex with antigens and fall out of solution from the blood. These immune complexes then deposit in body tissues inappropriately, and cause disease. This situation is especially noticeable in body tissues that have a direct filtering function. Which of the following structures would most likely be affected by a disease caused by immune complex deposition?
Hypersensitivity reactions occur when body tissues are affected by an abnormal immune reaction. The result is damage to normal tissues and clinical illness. A peanut allergy is an example of a hypersensitivity reaction, but there are three additional broad classes.
One class involves the abnormal production or deposition of antibodies. Antibodies are B-cell derived molecules that normally adhere to pathogens, rendering them unable to continue an infection. When antibodies are produced against normal tissues, however, disease can result. Figure 1 depicts a schematic structure of an antibody.
Antibodies can be divided into two peptide chains: heavy and light. Heavy chains form the backbone of the antibody, and are attached to light chains via covalent bonding. Each heavy and light chain is then further divided into constant and variable regions. Variable regions exhibit molecular variety, generating a unique chemical identity for each antibody. These unique patterns help guarantee that the body can produce antibodies to recognize many possible molecular patterns on invading pathogens.
In hypersensitivity reactions, antibodies can complex with antigens and fall out of solution from the blood. These immune complexes then deposit in body tissues inappropriately, and cause disease. This situation is especially noticeable in body tissues that have a direct filtering function. Which of the following structures would most likely be affected by a disease caused by immune complex deposition?
The glomerulus is the primary site of filtration in the kidney. Together, the glomerulus and Bowman's capsule for the renal corpuscle of the nephron and are responsible for collecting filtrate from the blood. Deposition and accumulation of immune complexes in the glomerulus would result in blockage of its filtering functions, impeding nephron function and preventing proper excretion of soluble wastes.
The sinoatrial node is the natural pacemaker region of the heart, located in the right atrium. Haversian canals are the central regions of osteons and often house nerves and blood vessels, facilitating cellular communication within bone. Neuromuscular junctions are the interface regions between a single neuron and the muscle fiber it innervates. The semicircular canals are located in the inner ear and function in the propagation an integration of sound vibrations. None of these structures are involved in filtration, and they would most likely be unaffected by the presence of immune complexes in the body.
The glomerulus is the primary site of filtration in the kidney. Together, the glomerulus and Bowman's capsule for the renal corpuscle of the nephron and are responsible for collecting filtrate from the blood. Deposition and accumulation of immune complexes in the glomerulus would result in blockage of its filtering functions, impeding nephron function and preventing proper excretion of soluble wastes.
The sinoatrial node is the natural pacemaker region of the heart, located in the right atrium. Haversian canals are the central regions of osteons and often house nerves and blood vessels, facilitating cellular communication within bone. Neuromuscular junctions are the interface regions between a single neuron and the muscle fiber it innervates. The semicircular canals are located in the inner ear and function in the propagation an integration of sound vibrations. None of these structures are involved in filtration, and they would most likely be unaffected by the presence of immune complexes in the body.
Compare your answer with the correct one above
Which of the following is not a function of the kidney?
Which of the following is not a function of the kidney?
The kidney is responsible for excreting nitrogenous waste produced by the urea cycle, maintaining water balance (and thus blood pressure), maintaining salt concentrations in the blood, and controlling blood pH by excreting or retaining protons. Blood flows into the nephrons through the glomerulus and is pushed into Bowman's capsule. The filtrate then flows through the proximal tubule, the main site for most reabsorption of glucose, proteins, and electrolytes. From the proximal tubule it enters the loop of Henle, where salt and water balance is regulated via the ion gradient in the extracellular space of the renal medulla. Finally, the filtrate enters the distal tubule and collecting duct, where salt, water, and proton balance is further regulates.
The liver is responsible for gluconeogenesis and glycogen storage.
The kidney is responsible for excreting nitrogenous waste produced by the urea cycle, maintaining water balance (and thus blood pressure), maintaining salt concentrations in the blood, and controlling blood pH by excreting or retaining protons. Blood flows into the nephrons through the glomerulus and is pushed into Bowman's capsule. The filtrate then flows through the proximal tubule, the main site for most reabsorption of glucose, proteins, and electrolytes. From the proximal tubule it enters the loop of Henle, where salt and water balance is regulated via the ion gradient in the extracellular space of the renal medulla. Finally, the filtrate enters the distal tubule and collecting duct, where salt, water, and proton balance is further regulates.
The liver is responsible for gluconeogenesis and glycogen storage.
Compare your answer with the correct one above
The proximal tubule of the nephron is the primary location for the reabsorption of which of the following blood filtrates?
The proximal tubule of the nephron is the primary location for the reabsorption of which of the following blood filtrates?
The proximal tubule of the nephron directly follows after Bowman's capsule, and is the first site of reabsorption. Any glucose and proteins that were able to enter the filtrate are removed here via active transport. Most glucose and proteins are blocked from the filtrate by the structure of the glomerulus wall and Bowman's capsule, but those that are able to pass must be removed quickly to maintain the proper oncotic pressures in the nephron. Sodium is perhaps the most important electrolyte in the body; though large quantities of sodium may enter the filtrate, over half of it is reabsorbed in the proximal tubule.
The proximal tubule also serves as a site for reabsorption for potassium and phosphate. Other regions of the nephron closely regulate the reabsorption of bicarbonate and protons, as well as fine-tune the balance of sodium and potassium.
The proximal tubule of the nephron directly follows after Bowman's capsule, and is the first site of reabsorption. Any glucose and proteins that were able to enter the filtrate are removed here via active transport. Most glucose and proteins are blocked from the filtrate by the structure of the glomerulus wall and Bowman's capsule, but those that are able to pass must be removed quickly to maintain the proper oncotic pressures in the nephron. Sodium is perhaps the most important electrolyte in the body; though large quantities of sodium may enter the filtrate, over half of it is reabsorbed in the proximal tubule.
The proximal tubule also serves as a site for reabsorption for potassium and phosphate. Other regions of the nephron closely regulate the reabsorption of bicarbonate and protons, as well as fine-tune the balance of sodium and potassium.
Compare your answer with the correct one above
The descending loop of Henle in the nephron is permeable to which of the following substances?
The descending loop of Henle in the nephron is permeable to which of the following substances?
The descending loop of Henle is responsible for the first step in urine concentration. Due to the high concentration of salt in the space surrounding the descending limb of the loop of Henle, water flows out of the tubule, concentrating the filtrate. The descending limb is impermeable to sodium, potassium, and albumin (the principle protein component in blood).
The descending loop of Henle is responsible for the first step in urine concentration. Due to the high concentration of salt in the space surrounding the descending limb of the loop of Henle, water flows out of the tubule, concentrating the filtrate. The descending limb is impermeable to sodium, potassium, and albumin (the principle protein component in blood).
Compare your answer with the correct one above